Contributed by Edward R. Marcantonio MD, MSc, Professor of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School and Donna M. Fick, RN, PhD, Director of the Center of Geriatric Nursing Excellence, Penn State
In 2020, we wrote a NIDUS blog introducing the Ultra-Brief Confusion Assessment Method (UB-CAM) 1, an ultra-brief, adaptive tool for assessing CAM-defined delirium 2. At the time, we had only preliminary results based on simulations using existing data sets 3, and small pilot studies 4. The purpose of this blog is to give an update on evidence from real-world implementation of the UB-CAM by clinicians, provide information about the availability of the UB-CAM app, and describe next steps.
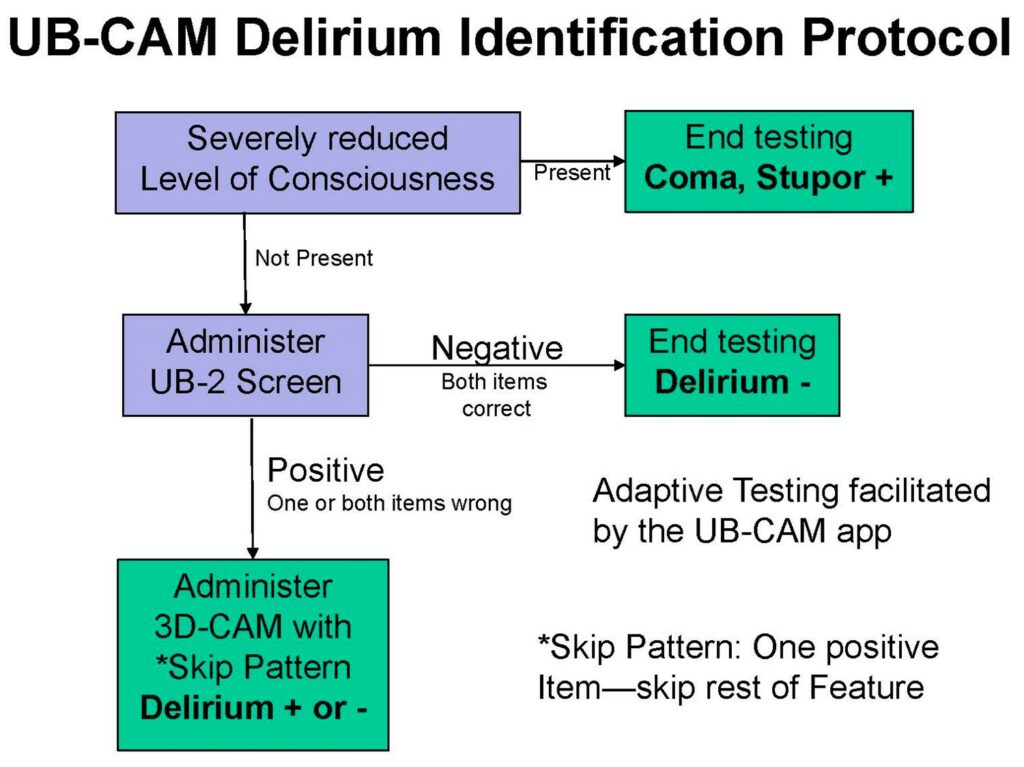
First, a brief review of the UB-CAM. The UB-CAM was created by combining the UB-2 Ultra-brief screen 5 with the 3D-CAM, a 3-minute diagnostic assessment for delirium 6. As depicted in Figure 1, the UB-2 begins with assessment of level of consciousness.
If severely reduced, then stupor or coma is present and the assessment ends. If stupor or coma are not present, the UB-CAM then administers the UB-2 Ultra-brief screen, which consists of two questions: 1) “Please tell me the months of the year backwards (to January), say December as your first month” (MOYB) and 2) “What is the day of the week? (DOW)”.
For DOW, the older adult may use orienting aids such as a white board, calendar, or newspaper. If the patient gets both MOYB and DOW correct, the assessment ends and delirium is not present. If the patient gets one or both of these questions incorrect (including no response or nonsensical responses) then the assessment proceeds with the 3D-CAM with skip pattern. The skip pattern is based on the 3D-CAM threshold of requiring 1 positive item to trigger the presence of a CAM Feature. For instance, if MOYB is incorrect (from the UB-2), this triggers the presence of Feature 2, Inattention, and the remainder of the Feature 2 items in the 3D-CAM can be skipped. This results in many fewer items being administered, which significantly shortens the duration of assessment.
In 2022, we reported on the comparative implementation of the UB-CAM by physicians, nurses, and certified nursing assistants (CNAs) as part of the READI: Researching Efficient Approaches to Delirium Identification study 7. READI was conducted at 2 hospitals and involved 527 general medicine inpatients and 399 clinicians. The patients were purposefully enrolled to be a “challenge population” with average age of 80 and over one-third having Alzheimer Disease and Related Dementias (ADRD).
Enrolled clinicians received brief training in the UB-CAM app—20-30 minutes for nurses and physicians, and less than 10 minutes for CNAs, who administered only the UB-2 screen. UB-CAM administration was integrated into routine care, and the results of clinician UB-CAMs were compared to a reference standard conducted by highly trained research associates, who performed a 45-minute assessment involving detailed patient cognitive testing, interviews with a family caregiver to assess changes from baseline, and medical record review.
We found that delirium identification using the UB-CAM was feasible, with 97% completion in 924 screening days (over 2700 days considering the 3 clinical disciplines). It was brief, taking on average one minute 20 seconds to complete, and under 50 seconds for the nearly two-thirds of patients who screened out at the UB-2 step.
The UB-CAM was also accurate, with 89% agreement on the presence or absence of delirium compared to the reference standard, and with over 80% sensitivity for cases of moderate to severe delirium. Nurses and physicians were equally fast and accurate, and CNAs were able to administer the UB-2 screen effectively (they did not perform the full UB-CAM since diagnosis is not in their scope of practice). The UB-CAM also worked well in patients with ADRD.
We also conducted qualitative research using both brief exit interviews with clinicians following UB-CAM screens and in-depth interviews with key informants at the conclusion of the study 8. Despite high workload in the inpatient setting, the clinicians were appreciative of the UB-CAM app, and particularly liked the use of technology to shorten the assessment while still providing a rigorous CAM-based diagnosis of delirium.
They also noted challenges, such as the noise and distractions of the inpatient setting, and the need to integrate delirium screening into regular workflow, including collection of “vital signs”. We also conducted an economic analysis 9, which found the cost of a single UB-CAM screen conducted by a nurse was only $1.66, and the annual costs for implementing a hospital-wide delirium identification program in a 300-bed hospital would be less than the average annual salary of the discipline performing the assessments.
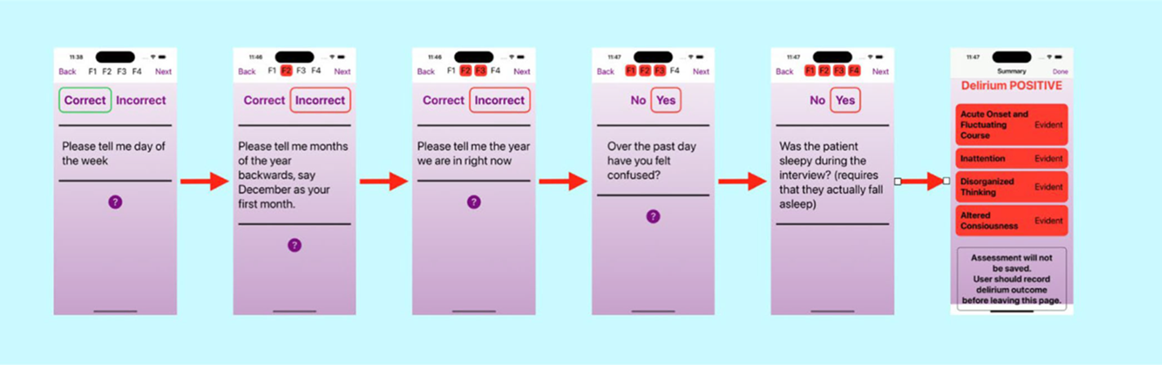
What have we done since completing the READI study? First, we have programmed the UB-CAM app, which was originally developed as a REDCap API 10, into both iOS and Android languages 11, and have released these free of charge on both the Apple and Google Play stores (the latter currently in process). Screen shots from the iOS app are shown below in Figure 2.

Scan this QR code to access the app in the Apple store.
We look forward to you downloading it and providing us with feedback—send to UBCAM@bidmc.harvard.edu. We continue to improve and expand the app, and will soon add recommendations for prevention or management, based on best practices, and customized to the app determination of delirium presence. We will also be translating the app into multiple languages.
We are currently launching our next project, READI-SET-GO: READI—Sustaining Effective Translation to create Gero-friendly Organizations. READI-SET-GO will be a test of full-scale implementation of UB-CAM delirium identification at three hospitals in Pennsylvania and Massachusetts, in which every patient over age 70 will be assessed at least daily using the UB-CAM, which will be integrated into the Electronic Health Record. We will again measure accuracy, and impact of systematic delirium identification (followed by best practice management) on patient and caregiver centered outcomes.
In summary, there is a large and growing body of evidence supporting delirium identification using the UB-CAM. We believe strongly that identification is the first key step in appropriate delirium management, and that implementation of the UB-CAM will be an important component of a systematic delirium intervention program to improve the outcomes of vulnerable, hospitalized older adults.
References
- Marcantonio ER, Fick DM, Jones RN, Inouye SK. The Ultra-Brief Confusion Assessment Method (UB-CAM): A New Approach for Rapid Diagnosis of CAM-Defined Delirium. NIDUS Blog. August 2020. https://deliriumnetwork.org/the-ultra-brief-confusion-assessment-method-ub-cam/
- Inouye SK, Van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: The Confusion Assessment Method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948. doi: 10.7326/0003-4819-113-12-941
- Motyl CM, Ngo L, Zhou W, et al. Comparative Accuracy and Efficiency of Four Delirium Screening Protocols. J Am Geriatr Soc. 2020;68(11):2572-2578. doi: 10.1111/jgs.16711
- Fick DM, Inouye SK, McDermott C, et al. Pilot Study of a Two-Step Delirium Detection Protocol Administered By Certified Nursing Assistants, Physicians and Registered Nurses. J Gerontol Nurs. 2018;44(5):18-24. doi: 10.3928/00989134-20180302-01
- Fick DM, Inouye SK, Guess J, et al. Preliminary development of an ultra-brief 2-item bedside test for delirium. J Hosp Med. 2015;10(10):645-650. doi: 10.1002/jhm.2418
- Marcantonio ER, Ngo L, O’Connor MA, et al. 3D-CAM: Validation of a 3-Minute Diagnostic Interview for CAM-defined Delirium. Ann Int Med. 2014;161(8):554-561. doi: 10.7326/M14-0865
- Marcantonio ER*, Fick DM* (*co-first), Jung Y, et al. Comparative Implementation of a Brief App-Directed Protocol for Delirium Identification by Hospitalists, Nurses, and Nursing Assistants: A Cohort Study. Ann Intern Med. 2022;175(1):65-73. doi: 10.7326/M21-1687
- Husser EK, Fick DM, Boltz M, et al. Implementing a Rapid, Two-Step Delirium Screening Protocol in Acute Care: Barriers and Facilitators. J Am Geriatr Soc. 2021;69(5):1349-1356. doi: 10.1111/jgs.17026
- Leslie DL*, Fick DM* (*co-first), Moore A, et al. Comparative salary-related costs of a brief app-directed delirium identification protocol by hospitalists, nurses, and nursing assistants. J Am Geriatr Soc. 2022;70(8):2371-2378. doi: 10.1111/jgs.17789
- Armstrong B*, Habtemariam D* (*co-first), Husser E, et al. A mobile app for delirium screening. JAMIA Open. 2021;4(2):ooab027. doi: 10.1093/jamiaopen/ooab027
- Kuzmik A, Hannan J, Boltz M, et al. A pilot study testing the iOS UB-CAM delirium app. J Am Geriatr Soc. 2023;71(6):1999-2002. doi: 10.1111/jgs.18252
Suggested Citation:
Marcantonio, Edward; and Fick, Donna. Update on the Ultra-Brief Confusion Assessment Method (UB-CAM), Network for Investigation of Delirium: Unifying Scientists (NIDUS); August, 2023, Available at: https://deliriumnetwork.org/update-on-the-ultra-brief-confusion-assessment-method-ub-cam/ (accessed today’s date)