Contributed by Gen Shinozaki, MD, Associate Professor of Psychiatry and Behavioral Health, Stanford University School of Medicine, Palo Alto, CA

Dr. Gen Shinozaki demonstrating a novel portable EEG device.
The Shinozaki Lab at Stanford University, previously at the University of Iowa, has been working to develop a novel portable EEG device to help detect delirium in hopes it will improve patient outcome(s). This bispectral EEG (BSEEG) device incorporates a single channel that is applied to the patient’s forehead (Figure 1). The BSEEG uses an algorithm to process the raw EEG patterns it captures over each 3-10 minute application to detect delirium based on the assumption that low-frequency (slow) brainwaves are present during periods of delirium.
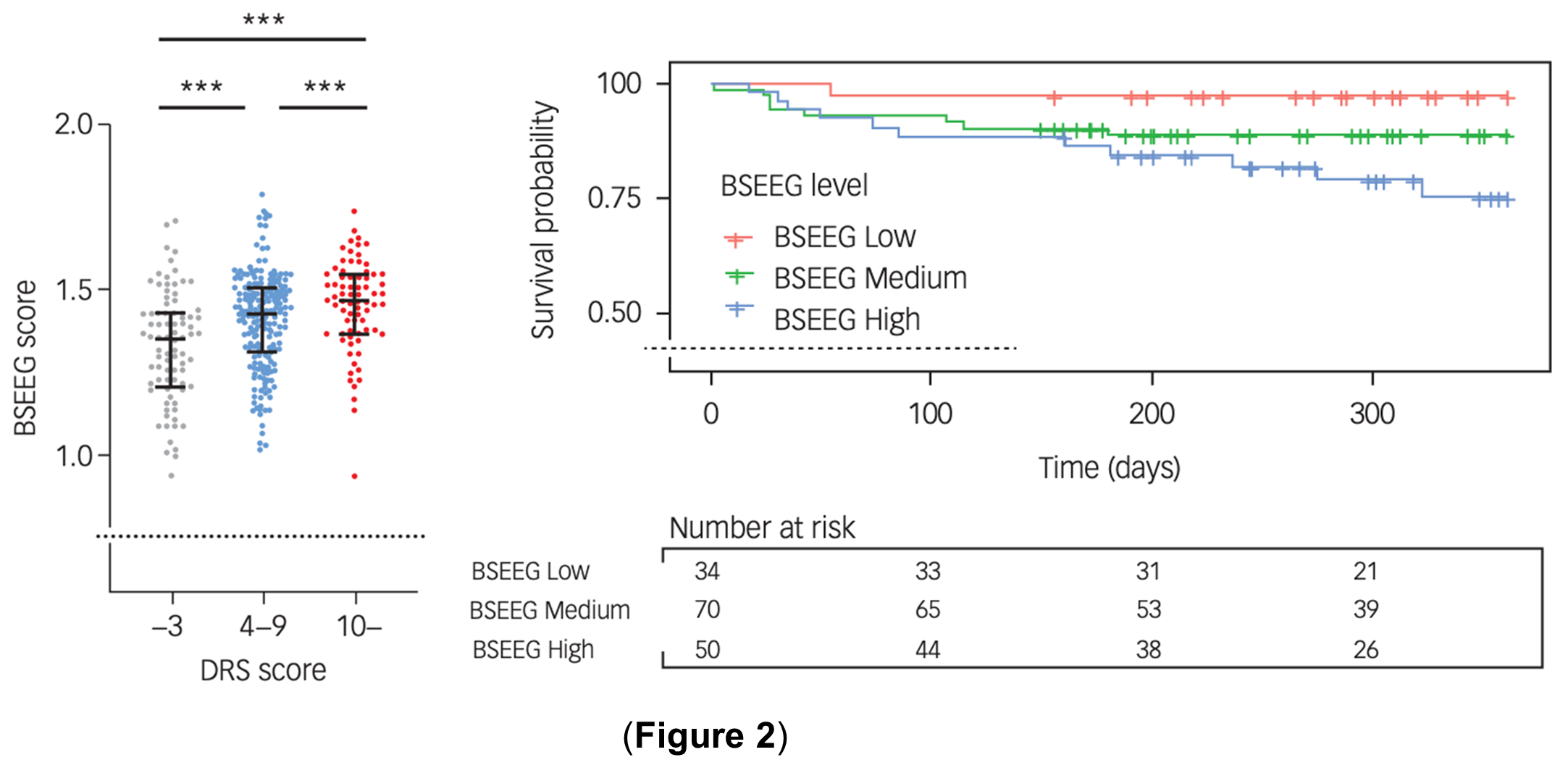
In 2018, our first study showed the application of the bispectral EEG (BSEEG) method was effective in detecting delirium (AUC >0.8) 1. To the best of our knowledge, this is the first published study demonstrating the effectiveness of a portable EEG device for delirium detection. Following this work, in 2019, our group demonstrated that a one-time BSEEG score recorded soon after admission to the hospital was able to effectively predict patient outcomes including one-year mortality, independent of the clinical diagnosis of delirium 2. Our group has also shown the usefulness of BSEEG in the context of dementia 3 as well as sepsis 4. In 2021, we demonstrated that a smaller thumb-size EEG device can generate BSEEG scores. In a subsequent study that employed this device, we found that a higher BSEEG score (indicative of having a greater slow frequency component in their brain wave) was associated with both delirium severity and mortality (Figure 2) 5.
Important unanswered questions remained from this prior research including the generalizability of the BSEEG methods regardless of age, independent of motor subtypes of delirium, and across different device types and settings. In this Blog, we would like to summarize our recent paper published in the American Journal of Geriatric Psychiatry 6 that addresses some of these remaining questions. We sought to establish a reliable and generalizable tool for identifying patients at high risk for poor outcomes.
To achieve our objective, we employed the following approach. We calculated a normalized BSEEG (nBSEEG) score from raw BSEEG data obtained in different cohorts from our previous investigations 2, 3, 5, encompassing a total of 1,077 subjects. These subjects were then categorized into three groups based on the nBSEEG score; low, middle and high.
The high nBSEEG score group represents patients having a greater slow frequency component in their brain wave signals. The study utilized log-rank tests and Cox proportional hazards models to assess patient survival at both 90-day and 1-year intervals.
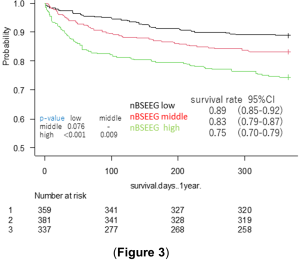 The result showed that the nBSEEG score had a clear association with a dose-dependent increase in mortality (after adjusting for covariates such as age, sex, Charlson Comorbidity Index, and delirium status. In short, the high nBSEEG group consistently exhibited significantly higher mortality than the middle nBSEEG group, and the middle group showed significantly higher mortality than the low nBSEEG group (Figure 3) 6.
The result showed that the nBSEEG score had a clear association with a dose-dependent increase in mortality (after adjusting for covariates such as age, sex, Charlson Comorbidity Index, and delirium status. In short, the high nBSEEG group consistently exhibited significantly higher mortality than the middle nBSEEG group, and the middle group showed significantly higher mortality than the low nBSEEG group (Figure 3) 6.
The results were similar across patient age groups. The hypoactive group showed the same results. The hyperactive group showed the same trend, although it did not reach a statistical significance likely due to its small sample size. The BSEEG method demonstrated its potential to effectively predict patient mortality and identify those at high risk of adverse outcomes.
The results of our study may have important clinical applications. By offering an objective and easily implementable method for detecting delirium and predicting patient outcomes, the BSEEG technology may help address the current challenges of delirium underdiagnosis in clinical settings. Future research needs to evaluate whether the use of BSEEG technology may help shorten the time to the initiation of interventions focused on reducing delirium and whether this improves patient outcomes and reduces healthcare costs. Our study also sheds light on the role of BSEEG in different age groups and delirium motor subtypes. The fact that the BSEEG method remained effective across these variables suggests its versatility and applicability across diverse patient settings.
The process by which this BSEEG technology can be best brought to the bedside requires further exploration. It is vital that this approach is user-friendly for clinicians and well-tolerated by patients. In an attempt to reach these goals, we intentionally avoided using multiple electrodes and their placement other than on a forehead, which could make this approach intolerable to patients, particularly if overnight, longer-term, recording is required in case of particularly high-risk patients such as those after major surgery.
In conclusion, our study underscores the potential utility and promise of using a single-channel BSEEG method to evaluate brain activity in patients at risk for delirium and poor outcomes. With the potential to accurately identify patients at high risk for poor outcomes including mortality, this technology could usher in a new era of personalized and targeted interventions for delirium and its associated complications.
Disclosure: Patents related to these BSEEG technologies have been filed. Dr. Shinozaki has co-founded a startup company (Predelix Medical) to bring this technology to market.
References
- Shinozaki G, Chan AC, Sparr NA, et al. Delirium detection by a novel bispectral electroencephalography device in general hospital. Psychiatry Clin Neurosci. 2018;72(12):856-863. doi: 10.1111/pcn.12783
- Shinozaki G, Bormann NL, Chan AC, et al. Identification of Patients With High Mortality Risk and Prediction of Outcomes in Delirium by Bispectral EEG. J Clin Psychiatry. 2019;80(5):19m12749. doi: 10.4088/JCP.19m12749
- Saito T, Malicoat JR, Leyden LR, et al. Mortality prediction by bispectral electroencephalography among 502 patients: its role in dementia. Brain Commun. 2021;3(2):fcab037. doi: 10.1093/braincomms/fcab037
- Yamanashi T, Mara PS, Crutchley KJ, et al. Mortality among patients with sepsis associated with a bispectral electroencephalography (BSEEG) score. Sci Rep. 2021;11(1):14211. doi: 10.1038/s41598-021-93588-9
- Yamanashi T, Crutchley KJ, Wahba NE, et al. Evaluation of point-of-care thumb-size bispectral electroencephalography device to quantify delirium severity and predict mortality. Br J Psychiatry. 2021;220(6):322-329. doi: 10.1192/bjp.2021.101
- Nishizawa Y, Yamanashi T, Saito T, et al. Bispectral EEG (BSEEG) Algorithm Captures High Mortality Risk Among 1,077 Patients: Its Relationship to Delirium Motor Subtype. Am J Geriatr Psychiatry. 2023;31(9):704-715. doi: 10.1016/j.jagp.2023.03.002
Suggested Citation
Shinozaki, Gen. Can Delirium Assessment with Bispectral EEG (BSEEG) Help Predict Patient Outcome(s)? , Network for Investigation of Delirium: Unifying Scientists (NIDUS); September, 2023, Available at: https://deliriumnetwork.org/can-delirium-assessment-with-bispectral-eeg-bseeg-help-predict-patient-outcomes/ (accessed today’s date)